Pain Management in Lupus
This site is intended for healthcare professionals as a useful source of information on the diagnosis, treatment and support of patients with lupus and related connective tissue diseases.
Introduction
Rheumatological disease is a major cause of increased morbidity and has a significant impact on the quality of life. Systemic Lupus Erythematous (SLE) is an autoimmune rheumatological disease, which is persistent and affects the muscles, joints and various other body parts. 90% of individuals will suffer from arthritis during their disease course.According to the International Association for the Study of Pain (IASP), pain is defined as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage, or both.”
Chronic pain is defined as pain, which is persistent and lasts 3 months beyond the healing process of an acute injury or illness. Pain is subjective, complex and it affects the emotional and cognitive responses of a person. Chronic pain prevalence increases with age and its sufferers report problems with normal activities of daily living. They have difficulty in sleeping, which in turn can cause increased daytime fatigue and drowsiness, difficulty in concentration and mood disturbances. It has a significant financial impact on not only the sufferer but also their families.
Pain in SLE
It is multifactorial and it is important to determine whether it is due to the active inflammation during a flare up or due to secondary causes. SLE causes pain due to inflammatory arthritis, tendonitis, serositis, peripheral neuropathy or painful skin lesions. The secondary causes of pain are due to developing chronic widespread pain syndromes such as Fibromyalgia, which is common, Chronic Fatigue Syndrome, Migraine, Avascular Necrosis of bone (AVN), Osteoarthritis or Vitamin D deficiency.Principles of Pain Management
It is a multimodal and multidisciplinary approach – involving rheumatologists, orthopaedic surgeons, pain physicians, GPs, physiotherapists, occupational therapists, psychologists and clinical nurse specialists specializing in pain management. The focus of chronic pain management is educating the patient and their family on the bio-psycho-social model of pain. This model embraces a holistic approach to pain management in long-term sufferers where their psychosocial and behavioural components are managed along with the physical pain and these factors often exaggerate their pain symptoms.Objectives are:
• Pain reduction
• Improve quality of life, mobility and independence
• Enhance the psychological well-being of the patient
Pharmacological methods of Pain Management:
• Medication (WHO analgesic ladder)
• Specific anti-inflammatory treatment for active SLE flare-ups
• WHO analgesic ladder for secondary pain
• Interventions (injections, denervation, implants)
Non-pharmacological methods of Pain Management:
• Physiotherapy
• Psychotherapy
• Complementary therapy
• Pain management program (PMP)
• Patient education and support groups
Treatment of Active Pain
The Rheumatologist best manages treatment of pain due to inflammatory arthritis during an active phase. The drugs, which may be used, are hydroxychloroquine and nonsteroidal anti-inflammatory drugs. For severe cases, steroids and immunosuppressant drugs such as methotrexate, azathioprine, mycophenolate and/or other biological drugs are used. The choice always has to take into account coexisting manifestations of SLE as well as co-existing other disease and risk factors, especially relating to renal and cardiac disease. If pain is due to AVN, an orthopaedic opinion is helpful as the patient may benefit from surgery.Secondary pain management with medication
World Health Organization (WHO) introduced a 3-step ladder for cancer pain in 1986, which was extended to non cancer pain. It worked well for acute pain but had limitations for its use for chronic pain. The main recommendations of the ladder were that analgesic therapy should be individualized to patients and medications should be administered orally and on a regular basis. This was later modified to include a fourth step to incorporate interventional therapies wherever possible, within guidelines, and to add adjuvant therapies whenever possible (see Table 1). For mild pain, simple painkillers include paracetamol and non-steroidal antiinflammatory drugs (NSAIDs) such as Ibuprofen and Naproxen. Weak opioids like codeine and simple analgesics from step 1 can be administered for moderate pain and strong opioids are reserved for severe pain. At all stages adjuvant drug therapy should be considered as it helps manage the pain better with limiting theside-effects of the analgesics. Adjuvant therapy includes antineuropathic drugs such as anticonvulsants, antidepressants, anxiolytics and miscellaneous drugs.

Paracetamol
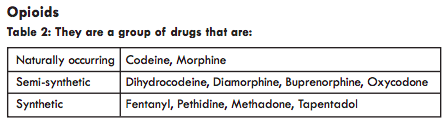
They exhibit their actions by acting on different types of opiate receptors.
Main pharmacological effects of opioids are analgesia, euphoria and sedation, respiratory depression and suppression of cough, nausea and vomiting, reduced gastrointestinal motility, histamine release and pupillary constriction.
Weak opioids
Codeine Oral 30-60mg four times a day. It is reliably absorbed orally with, little or no euphoria but patients frequently complain of constipation. 10% of population is unresponsive (Co-codamol is a combination prescription of codeine 8mg or 30mg + paracetamol 500mg) Dihydrocodeine Oral (DF118 Forte, DHC Continus)
Strong opioids
Buprenorphine Sublingual, Transdermal (Temgesic, Transtec, BuTrans) Diamorphine (Heroin) Oral Fentanyl Transdermal, Transmucosal oral (Duragesic, Actiq) Hydromorphone Oral (Palladone, Palladone SR) Methadone Oral Morphine Oral (Oramorph, Sevredol, MST Continus, MXL, Zomorph). Morphine is the prototype opioid and has a higher affinity for MOP receptors hence effective analgesia. It is the most commonly prescribed. Oxycodone Oral (OxyNorm, OxyContin); twice as potent as morphine Oxycodone +Naloxone (Targinact) Pethidine Oral 50-100mg four times a day. It is hallucinogenic and convulsant and is commonly used in labour Tramadol* Oral 50-100mg four times a day (Zydol, Zamadol). It is a centrally acting opioid agonist and has a dual mode of action by inhibiting noradrenaline reuptake. It has some evidence in Fibromyalgia.
Opioid conversion
Morphine - 30mg Oromorph = 20mg MST/day
Codeine - 240mg = 30mg Morphine/day
Fentanyl – 25mcg/h patch = 90mg Morphine/day
Buprenorphine – 5mcg/h patch = 8mg Morphine/day
Tramadol - 400mg = 40 to 80mg morphine/day
Oxycodone - 10 mg = 20mg Morphine/day
Methadone- 1mg = 2-8mg Morphine/day
Adverse effects of Opioids
80% of the patients will experience at least one adverse effect. Commonest ones are constipation, nausea, somnolence, itching, dizziness, vomiting. Respiratory depression can occur with high doses, change in dose, formulation, route or accidental overdose.
Long term side-effects of Opioids Hormonal effects causing increase in circulating prolactin, decrease in LH, FSH, testosterone and oestrogen. These changes lead to a decrease in libido and fertility, amenorrhoea, irregular menses and weight gain.
Immunological effects - Opioids alter the development of immune cells, and bone marrow cell lines, macrophages, natural killer cells, and T and B lymphocytes are all affected. The patients’ immunity is decreased and the risk of infections is increased.
Opioid induced hyperalgesia (OIH) occurs with prolonged use. It is associated with increased pain that is diffuse and less defined in quality. Such patients are managed by dose reduction or opioid swapping.
Central nervous system - Drowsiness usually settles after initial period but may impair performance. Cognitive impairment from opioids potentially interferes with daily functioning and driving ability.
Over time patients develop tolerance to the drug, which leads to increasing dose for the same effect, dependence on the medication and addiction.
Opioids and Driving
Patients should be made aware to avoid driving if they feel unfit to drive, have just started treatment, recently adjusted dose, consumed alcohol or their condition has physical consequences that might impair their driving ability Responsibility rests with the patient to inform the DVLA if they have any concerns.
Opioids do provide useful analgesia in the short and medium term but are rarely able to provide complete relief of pain. The goal should be to reduce pain sufficiently to facilitate engagement in rehabilitation.
‘Opioid Aware’ a resource by Public Health England - “The risk of harm increases substantially at doses above an oral morphine equivalent of 120mg/day, but there is no increased benefit”.
Main pharmacological effects of opioids are analgesia, euphoria and sedation, respiratory depression and suppression of cough, nausea and vomiting, reduced gastrointestinal motility, histamine release and pupillary constriction.
Weak opioids
Codeine Oral 30-60mg four times a day. It is reliably absorbed orally with, little or no euphoria but patients frequently complain of constipation. 10% of population is unresponsive (Co-codamol is a combination prescription of codeine 8mg or 30mg + paracetamol 500mg) Dihydrocodeine Oral (DF118 Forte, DHC Continus)
Strong opioids
Buprenorphine Sublingual, Transdermal (Temgesic, Transtec, BuTrans) Diamorphine (Heroin) Oral Fentanyl Transdermal, Transmucosal oral (Duragesic, Actiq) Hydromorphone Oral (Palladone, Palladone SR) Methadone Oral Morphine Oral (Oramorph, Sevredol, MST Continus, MXL, Zomorph). Morphine is the prototype opioid and has a higher affinity for MOP receptors hence effective analgesia. It is the most commonly prescribed. Oxycodone Oral (OxyNorm, OxyContin); twice as potent as morphine Oxycodone +Naloxone (Targinact) Pethidine Oral 50-100mg four times a day. It is hallucinogenic and convulsant and is commonly used in labour Tramadol* Oral 50-100mg four times a day (Zydol, Zamadol). It is a centrally acting opioid agonist and has a dual mode of action by inhibiting noradrenaline reuptake. It has some evidence in Fibromyalgia.
Opioid conversion
Morphine - 30mg Oromorph = 20mg MST/day
Codeine - 240mg = 30mg Morphine/day
Fentanyl – 25mcg/h patch = 90mg Morphine/day
Buprenorphine – 5mcg/h patch = 8mg Morphine/day
Tramadol - 400mg = 40 to 80mg morphine/day
Oxycodone - 10 mg = 20mg Morphine/day
Methadone- 1mg = 2-8mg Morphine/day
Adverse effects of Opioids
80% of the patients will experience at least one adverse effect. Commonest ones are constipation, nausea, somnolence, itching, dizziness, vomiting. Respiratory depression can occur with high doses, change in dose, formulation, route or accidental overdose.
Long term side-effects of Opioids Hormonal effects causing increase in circulating prolactin, decrease in LH, FSH, testosterone and oestrogen. These changes lead to a decrease in libido and fertility, amenorrhoea, irregular menses and weight gain.
Immunological effects - Opioids alter the development of immune cells, and bone marrow cell lines, macrophages, natural killer cells, and T and B lymphocytes are all affected. The patients’ immunity is decreased and the risk of infections is increased.
Opioid induced hyperalgesia (OIH) occurs with prolonged use. It is associated with increased pain that is diffuse and less defined in quality. Such patients are managed by dose reduction or opioid swapping.
Central nervous system - Drowsiness usually settles after initial period but may impair performance. Cognitive impairment from opioids potentially interferes with daily functioning and driving ability.
Over time patients develop tolerance to the drug, which leads to increasing dose for the same effect, dependence on the medication and addiction.
Opioids and Driving
Patients should be made aware to avoid driving if they feel unfit to drive, have just started treatment, recently adjusted dose, consumed alcohol or their condition has physical consequences that might impair their driving ability Responsibility rests with the patient to inform the DVLA if they have any concerns.
Opioids do provide useful analgesia in the short and medium term but are rarely able to provide complete relief of pain. The goal should be to reduce pain sufficiently to facilitate engagement in rehabilitation.
‘Opioid Aware’ a resource by Public Health England - “The risk of harm increases substantially at doses above an oral morphine equivalent of 120mg/day, but there is no increased benefit”.
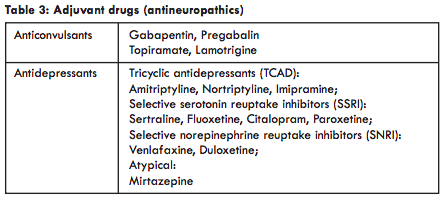
Gabapentinoids - Gabapentin
Its main use is as an antineuropathic, analgesic and anticonvulsant drug. It works by blocking the calcium channels after binding at a unique site at the voltage dependant Ca channels.The dose in adults is a maximum of 3600mg/day in three divided doses, although doses above 600mg, thrice a day (1800mg/day) should be avoided, as the effect of the drug is not much improved at higher doses. Starting dose should be 100mg, thrice a day and slowly increased as tolerated.
The common side-effects are dizziness, sedation, ataxia, nystagmus, headache, tremor, nausea, vomiting and in some patients can cause water retention and weight gain.
Orally, it has a bioavailability of 60% of the drug that is. This decreases with increasing doses. It is excreted unchanged in the urine, hence doses should be decreased in renal failure.
When used with opioids it has an opioid sparing effect and helps with pain management.
Gabapentinoids - Pregabalin
It is a second generation gabapentinoid and is very similar to Gabapentin. Maximum dose is 600mg/day but should be initiated at 75mg twice a day and slowly titrated up to tolerable doses. It is used for patients who cannot tolerate Gabapentin. Gabapentinoids have been misused for recreational purposes. If the patient does not gain benefit from the drug, it should be weaned down slowly and stopped.Antidepressants
These work by modulation of the descending inhibitory pain pathway through serotonin and norepinephrine reuptake inhibition, block the sodium and calcium channels and have some opioid action as well.Side-effects include dry mouth, constipation, micturition disturbance, sedation, orthostatic hypotension, cardiac conduction abnormalities. They should be used with caution in patients who have cardiovascular problems, urinary retention or glaucoma.
Amitriptyline/Nortriptyline - advantageous in patients who are struggling to sleep. Dose started at 10mg ca 3 hours before bedtime and slowly increased to a maximum of 75mg at night. In some patients it can work negatively and can increase risk of suicidality, somnolence, day time tiredness, dizziness and difficulty in concentration. Duloxetine has a dual antineuropathic and an antidepressant effect and can be started at 30mg once a day and increased to 60mg/day, single dose. The common side-effect is nausea/vomiting, but this commonly settles over time. It has FDA approval for Fibromyalgia, which is often existing in SLE patients. Topical treatment for focal neuropathic pain
• Capsaicin 8% patch is a specialized treatment offered under pain management team in hospital. It may not be well tolerated by the patient as the patch stays on for 30-60 minutes and has a very strong burning effect. It works by desensitizing TRPV-1 sensory axons to decrease polarization, initiation of an action potential and pain signal transmission.
• Lidocaine 5% patch is licensed for post herpetic pain only. The patch can be used in primary care and it stays on for 12 hours and off for 12 hours. It reduces spontaneous ectopic nerve discharge by antagonizing sodium channels and helps with localized neuropathic pain.
Interventions
Interventional therapy is helpful when pain is not adequately managed by pharmacological and nonpharmacological methods. They not only help in reducing pain and disability but also help in diagnosing the source of pain. They are not curative but assist in managing symptoms and not all pain is amenable to interventional therapy. They are performed as part of the multidisciplinary, holistic management of pain.They range from injections at a local site to blockade of nerves to specific body parts.
Interventional therapies usually need aids to precisely locate the injection sites. This may be in the form of Fluoroscopy, which requires a portable C- arm for X Rays, CT scan in the radiology department or Ultrasound machine and medications. These procedures need technical skills and have side-effects and risks associated with them. The risk depends on the level of invasiveness of the procedure and may vary from bleeding, risk of infection, damage to structures in the surrounding area including nerve damage or burns to the skin for denervation procedures.
The commonly used solution is local anaesthetic and steroids, which act as an antiinflammatory agent at the site.
This therapy is not suitable if patients do not have capacity to consent for the procedures, localized or systemic infection or bleeding disorders.
The common interventional therapies include
• Trigger point injections when there is myofascial pain and palpable triggers which cause referred pain.
• Medial branch blocks (MBB) for facet joint pain. This occurs more commonly in the lumbar and cervical region but can occur in the thoracic region too. The pain relief from these procedures can be short-lived but they can act as a diagnostic block and can be followed on with radiofrequency (RF) denervation, which can provide benefit for a longer period, from 6 months to 18-24 months, sometimes longer. Denervation involves electrical lesioning the medial branches if the patient has had benefit from the medial branch blocks.
• Sacroiliac joint injections and radiofrequency of the sacroiliac joints are
similar to MBBs and their RF denervation and can be offered for sacroiliac
joint pain to aid rehabilitation.
• Nerve root, epidural injections including caudal epidural is offered when
patients have radicular pain i.e. neuropathic pain down the distribution of
specific spinal nerves.
• Peripheral nerve blocks such as intercostal nerve blocks for localized rib pain or post herpetic neuralgia, suprascapular nerve block for shoulder pain, ilioinguinal nerve block for post hernia surgery pain.
• Specialized interventions such as spinal cord stimulators (SCS) and intrathecal drug delivery systems (ITDDs) are invasive procedures with very specific indications and require a long-term commitment from the patient.
Interventional therapy aids with symptom management and should be a part of the whole therapy package offered including physiotherapy.
Physiotherapy
This is an integral part of pain management especially in chronic conditions. Physiotherapy includes exercise, manual therapy, graded exercise therapy and education to reduce disability and restore movement and functionality. It helps with the rehabilitation in patients suffering with persistent pain. A very important part of rehabilitation is the focus on self management through awareness andeducation.
Pain management is achieved by release of endorphins centrally and activation of the descending inhibitory pain pathway, increasing the available serotonin, dopamine and norepinephrine. All these chemicals decrease pain and improve mood.
Exercise therapy is widely applied and the treatment is aimed to promote the well being of the patient. This includes core-strengthening exercises, improving muscle power and range of movements of joints. Individualized intensive manual therapy programs are much more helpful and beneficial to chronic pain sufferers.
Manual therapy incorporates active and passive movement of both major joints and the small joints of the spine to improve the range of movement.
Graded exercise therapy has a strong evidence base in Fibromyalgia decreasing disability and improving independence and function. As the name suggests, the therapy starts very gradually with stretching routines and slowly increases over time to strengthening exercises. It helps to address fear avoidance behaviours and build self-confidence by exercising in a guided, gradual fashion.
Hydrotherapy uses the buoyancy property and the warmth of water (30-35 degrees) for gentle exercise in a swimming pool. Warm water can be soothing and helps with relaxation in patients suffering from musculoskeletal pain. Exercising in water has the same advantages as land exercise but is better in rehabilitation as patients manage difficult exercise much more easily in warm water.
Functional Restoration program is a combination of physical and psychological treatment in patients suffering from back pain. It is specifically designed for patients who are struggling with normal daily activities but are motivated and want to adopt the self-management techniques.
Psychotherapy
Evidence has shown that depression affects pain negatively and vice-versa. SLE patients suffer from chronic pain on a regular basis and over time this can lead to frustration, anxiety about worsening condition and depression. The pain and worry lead to sleep disturbance, which in turn leads to day time tiredness and exhaustion and worsening pain. It is a vicious cycle and hence the need of a multidisciplinary approach targeting pain, sleep and mood disturbances.Along with medication for pain management, antidepressants such as duloxetine and tricyclic agent such as amitriptyline should be considered. Amitriptyline also helps with sleep. Relaxation techniques, music, prayer, meditation can be self-taught and have helped in decreasing the suffering caused by chronic pain.
Cognitive behaviour therapy (CBT) is very beneficial in management of the suffering caused by pain and helps improve coping skills. It is provided by CBT therapists and can be accessed through the GP. It works on recognizing the negative thoughts and beliefs which lead to unhelpful behaviours. CBT helps the patient adopt techniques that challenge the negative thinking and avoidance of activity in the fear of pain. NICE recognizes it as the choice of treatment of anxiety and depression.
Acceptance Commitment therapy (ACT) is another model of therapy which has been well studied, with promising results, in the management of chronic pain. The aim of ACT is to support patients who are willing to accept conditions that are not within their control. Once they can accept their condition, they have to commit to adopt strategies to make changes that enrich and make their life meaningful. This reduces the negative impact of pain on their lives.
Mindfulness is a type of therapy involving meditation and focus in the present moment in an open, flexible and non judgmental way. The process trains the patient to change how they experience what they think, feel and do rather than trying to change what they think and feel. It has good evidence in stress reduction and helps in pain management.
Hypnotic therapy has been used in pain management as it helps reduce anxiety and increases relaxation. It works on an altered level of conscious awareness where the patient opens up to suggestions to change their perception and behaviour. It is important to know that pain is neither physical pain nor psychological pain.
They are both involved in pain processing and it is important to recognize and understand this and reduce unhelpful behaviours.
Pain management program (PMP)
PMP is rehabilitative treatment approach for patients suffering with chronic pain. It does not aim to relieve pain but enables and empowers patients to cope and manage their pain better through education, physical and psychological therapy, decreasing distress and disability, thereby, improving their quality of life. It is run by a multidisciplinary group of healthcare professionals including doctors, nurses, therapists and psychologists.It is usually an interactive group therapy with 8 to 12 individuals. The duration recommended is 12 half-day sessions over 6-10 weeks. Intensive PMP aims to deliver the program over 15-20 whole days.
The main components are patient education, teaching coping and pacing strategies, (avoiding the ‘boom-bust’ cycle of overdoing things when pain is at a manageable level), skills training, goal setting and psychological interventions focusing mainly on improving function and independence.
Complementary and Alternative therapies (CAM)
Transcutaneous Electrical Nerve Stimulation (TENS) is a non-invasive technique that provides analgesia using electric currents, easily available in pharmacies without a medical prescription. The kit consists of electric pads, which are applied on the painful area with current generated by a hand held portable pulse generator. The dose and current can be adjusted by the patients themselves. The pads on the skin deliver low voltage electrical impulses, which in turn activate the small nerve fibres, superficially releasing neurotransmitters that inhibit pain transmission and decreasing the perception of pain by the ‘Gate control theory’. According to this theory, when the peripheral nerves are stimulated, the secondorder nociceptors or pain receptors are depressed in the spinal cord.Acupuncture involves placing fine acupuncture needles on the body, 4 25mm deep and left for a short period of time. Up to 12 needles are usually placed at one time and it can produce a tingling dull ache-like sensation. The mechanism of action may be, by improving blood flow locally to stimulate healing, release of endorphins or stimulation of the tissues which releases anti-inflammatory substances. It may also cause relaxation of muscle fibres by a local effect or the mechanism may be by the ‘Gate control theory’ mentioned above. The various other forms of acupuncture include electro-acupuncture where a small electric current is applied to the needle, which causes a non-painful twitching; laseracupuncture which uses the laser beam and acupressure.
In the UK, the other popular forms of complementary and alternative medicine are herbalism, aromatherapy, homeopathy, massage and reflexology. Vitamin D, magnesium, Vitamin C, turmeric and hemp seed oil are alternative forms of therapy that are gaining popularity and there is some emerging evidence that they may be helpful. Heat and cold therapy, traction, massage, yoga, chiropractic and osteopathy have all been used for management of chronic pain conditions.
In summary, pain in patients suffering with SLE can be chronic and debilitating. Secondary Fibromyalgia is commonly present along with arthritis pain. Management requires a multidisciplinary approach encompassing pharmacological and non-pharmacological methods to provide symptomatic relief, decreasing disability and improving the quality of life.
References:
1) Tsui SL, Chen PP, Ng KFJ. Pain Medicine, A multidisciplinary Approach. Hong
Kong University Press
2) Brook P, Connell J, Pickering T. Oxford Handbook of Pain Management.
Oxford University Press
3) https://www.e-lfh.org.uk/
Dr Alifia Tameem
Consultant Anaesthetics and Pain Management
Dudley Group NHS Foundation Trust
Russells Hall Hospital
Pensnett Road
Dudley
West Midlands, DY1 2HQ
1) Tsui SL, Chen PP, Ng KFJ. Pain Medicine, A multidisciplinary Approach. Hong
Kong University Press
2) Brook P, Connell J, Pickering T. Oxford Handbook of Pain Management.
Oxford University Press
3) https://www.e-lfh.org.uk/
Dr Alifia Tameem
Consultant Anaesthetics and Pain Management
Dudley Group NHS Foundation Trust
Russells Hall Hospital
Pensnett Road
Dudley
West Midlands, DY1 2HQ

 ©2024 LUPUS UK (Registered charity no. 1200671)
©2024 LUPUS UK (Registered charity no. 1200671)