Juvenile-Onset Lupus
This site is intended for healthcare professionals as a useful source of information on the diagnosis, treatment and support of patients with lupus and related connective tissue diseases.
Introduction
Although rare, juvenile-onset systemic lupus erythematosus (JSLE; also known as paediatric lupus, pSLE or childhood SLE, cSLE) causes significant morbidity and even mortality in children. It is a complex illness which can present with such a variety of symptoms and signs that it can mimic many common paediatric conditions. This means the diagnosis is often difficult to make and there are frequently significant delays in attaining specialist care. Much is inferred about the disease from adult-onset lupus, however, children are not mini-adults: their normal growth, development and evolving immune system affect the disease presentation and complicate its diagnosis and management.What is so special about JSLE?
• Severity of the disease - JSLE has a more severe disease presentation than lupus in adults, with a higher incidence of major organ involvement and a more aggressive disease course. Paediatric patients are more likely to die in the acute phase of the illness compared to adults who more commonly die of disease complications. However, JSLE patients will also have longer disease duration than their adult counterparts and so have a higher chance of developing complications.• Additional management challenges - Longer exposure time and reexposure to carcinogenic or gonadal-toxic agents are of particular importance to patients with JSLE. Handling and bioavailability of potent immune-modulating drugs differs between adults and children. Side effects of drugs used in the management of JSLE can be particularly problematic in adolescents with JSLE. JSLE can have a dramatic impact on a child’s education, social development and, indeed, their whole family.
How common is JSLE?
• There are no robust incident data for JSLE in the UK, although this is currently being investigated as part of a British Paediatric Surveillance Unit study seeking to identify all new patients diagnosed with JSLE across the UK and Ireland, that is supported by LUPUS UK.• Data from different ethnic populations from around the world put the incidence between 0.5 and 6 per 100,000.
• Approximately 15-20% of patients with lupus will present in childhood or adolescence.
• The female predominance of lupus found in adults is less apparent in JSLE. While the overall female to male ratio in JSLE is approximately 4.5:1, this difference is even less marked pre-puberty.
• Children of any age can develop JSLE, although it is extremely rare before the age of 5 years.
Challenges of diagnosing JSLE
• Clinical manifestations of JSLE are extremely variable, from a relatively mild disease characterised by facial rash, joint pains and fatigue, to a severe lifethreatening illness.• These non-specific features can make JSLE a major diagnostic conundrum. Knowledge and experience of the spectrum of paediatric and adolescent disease and awareness of classification criteria for SLE can help the clinician to consider a diagnosis of JSLE and instigate further investigations and referral to a specialist paediatric centre.
• The symptoms of JSLE may not all occur at the same time. They may occur sequentially. Patients may have already been diagnosed with another condition such as chronic fatigue, juvenile idiopathic arthritis and idiopathic thrombocytopenia. Careful monitoring and comprehensive re-evaluation of the patient’s past history may be necessary in order for the diagnosis of JSLE to be made.
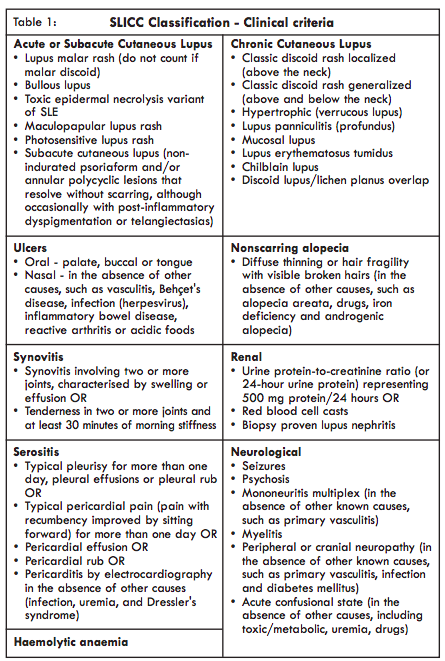
Classification criteria for JSLE
• The 2017 SHARE (Single Hub and Access point for paediatric rheumatology in Europe) recommendations for diagnosis and treatment of childhood SLE [1] advocate use of the 2012 Systemic Lupus International Collaborating Clinics (SLICC) classification criteria for SLE in JSLE [2]. These classification criteria have been shown to have better sensitivity than the American College of Rheumatology (ACR) criteria in JSLE, which can also still be used. The SLICC classification criteria can be used to aid referral to, or at least consultation, with a paediatric rheumatologist.• The SLICC criteria require ≥ 4 criteria (including at least 1 clinical and 1 immunological criteria), or biopsy proven LN with positive antinuclear (ANA) or anti-double stranded DNA (anti-dsDNA) antibodies.
• To improve early referral to paediatric rheumatology care the SHARE recommendations state that referral to paediatric rheumatology should be considered even if a child does not fulfil ≥ 4 criteria, and particularly if exhibiting a positive ANA combined with:
o 2 clinical SLICC criteria
o 1 clinical and 1 immunological SLICC criterion
• The SLICC classification criteria for SLE are shown in Table 1 below. The ACR classification criteria can be found on page Specific Symptoms.
• An on-line calculator can be used to help calculate the SLICC score (see
https://qxmd.com/calculate/calculator_274/slicc-sle-criteria)
differential diagnosis
• The differential diagnosis of JSLE is extensive and includes infection, malignant disease, other auto inflammatory conditions and any specific organ-associated disease. The ability to diagnose JSLE correctly, particularly in the adolescent, may be very challenging and require great clinical acumen.Major organ involvement
This must be actively sought and excluded. Renal, neuropsychiatric and haematological involvement occurs more frequently in JSLE.• Neuropsychiatric lupus, a cause of debilitating long-term morbidity in JSLE, can be very difficult to diagnose and can manifest in a vast range of presentations including headache, depression, severe anxiety, aseptic meningitis, seizures, psychosis, visual disturbance or visual loss. Importantly, a normal MRI does not exclude neuropsychiatric lupus. Impairment of cognition, with difficulties with memory and concentration tasks and declining school performance, has also been observed in JSLE.
• Nephritis is much more common at diagnosis in JSLE than in adults. Proteinuria in an early morning urine or mild hypertension may be the only initial manifestations of significant renal involvement. However, patients may also present with severe hypertension, nephritic syndrome or acute renal failure. Urinalysis at every clinical encounter is crucial as patients with Lupus Nephritis may be entirely asymptomatic. Prompt treatment improves renal outcomes.
• As with adult-onset lupus, JSLE can affect any organ system in many different ways. Cardiopulmonary manifestations are increasingly recognised in JSLE and routinely screened for at diagnosis.
Access of specialist services - Arthritis and Musculoskeletal Alliance (ARMA) Guidelines
• Early diagnosis and access to specialist services can significantly improve outcome and reduce the risk of life threatening events. Patients, unfortunately, frequently attend numerous appointments and specialists before a diagnosis is finally made.• Recently published ARMA guidelines stipulate that GPs should have access to specialist units where assessment can be made by a multi-disciplinary team led by a paediatric rheumatologist. Each local District General Hospital should have a nominated paediatrician with knowledge of paediatric rheumatology including JSLE, access to, and regular communication with, regional specialist centres to whom they can refer on where appropriate. Emergency services should, therefore, be available for specialised connective tissue disease advice.
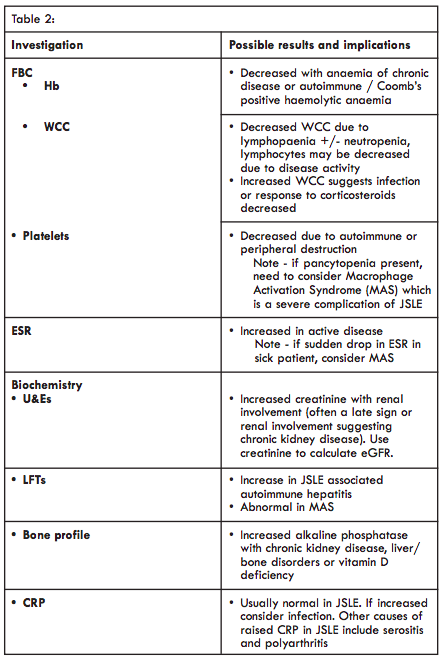
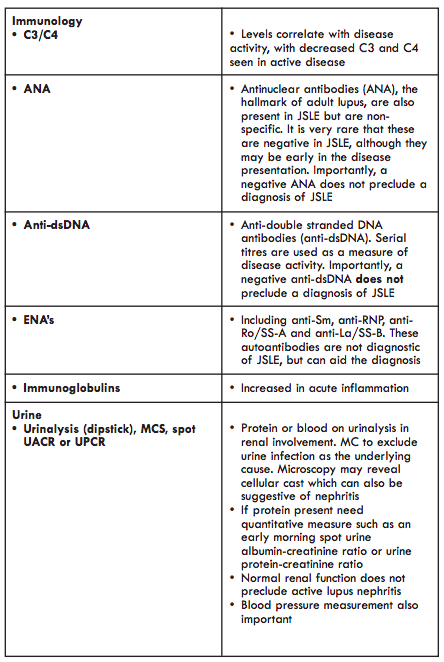
Interpretation of investigations and differential diagnoses
• As with adult-onset disease, there is no one diagnostic test for JSLE. All routine tests to aid the diagnosis (and long term monitoring of disease activity) are non-specific. They must be interpreted in the context of the clinical features and other bio-markers.• The differential diagnosis of JSLE is extensive and includes infection, malignant disease, other auto-inflammatory conditions and any specific organassociated disease. The ability to diagnose JSLE correctly, particularly in the adolescent, may be very challenging and require great clinical acumen.
Appropriate speed and referral pathway
• All children who are systemically unwell, have signs of major organ involvement, are clinically deteriorating or are not responding to existing therapy should be referred as an emergency for further investigation and assessment.• Any child suspected of having JSLE should be discussed with or referred to a paediatrician or paediatric rheumatologist as soon as possible.
Access of specialist services – Arthritis and Musculoskeletal Alliance (ARMA) Guidelines
• Early diagnosis and access to specialist services can significantly improve outcome and reduce the risk of life-threatening events. Patients, unfortunately, frequently attend numerous appointments and specialists before a diagnosis is finally made.• Recently published ARMA guidelines stipulate that GPs should have access to specialist units where assessment can be made by a multi-disciplinary team led by a paediatric rheumatologist. Each local District General Hospital should have a nominated paediatrician with knowledge of JSLE, access to and regular communication with regional specialist centres to whom they can refer on where appropriate. Emergency services should, therefore, be available for specialised connective tissue disease advice.
Management of patients with JSLE
There is significant lack of evidence for therapeutic intervention specific to JSLE. Although much is inferred from case series or adult studies where the disease characteristics vary. There is now an impetus from national and international collaborations to perform randomised controlled trials in JSLE. The 2017 SHARE recommendations provide an internationally developed and evidence based, structured approach to the treatment (as well as diagnosis) of JSLE [1]. In addition, there are specific SHARE recommendations for the diagnosis and treatment of lupus nephritis in JSLE [3] and the associated complication of paediatric anti-phospholipid syndrome [4].• Immuno-suppressive therapies - Medications currently used to treat JSLE include: hydroxychloroquine; azathioprine or methotrexate for mild/moderate disease; mycophenolate mofetil or intravenous cyclophosphamide for severe disease or major organ involvement and, more recently, biologic therapies such as rituximab. Regular blood monitoring is important.
• Treatment of intercurrent infection - Patients with JSLE have an abnormal immune response as part of their disease process and all of the therapeutic agents used are associated with immuno-suppression. Any sign of infection must be actively investigated and aggressively treated. If a patient with known JSLE presents to primary care with an intercurrent illness, then liaison with their lead team should take place.
• Sunblock - The highest factor sunblock is important, even on cloudy days.
• Multi-disciplinary care - Patients with JSLE should receive multidisciplinary care from professionals trained to address the diverse and complex issues of a chronic paediatric multi-system disease. This input is vital to address their considerable needs and concerns.
Integration of patient care in JSLE
Integration of care across primary, secondary and tertiary services is vital to improving outcome and to support children and adolescents with JSLE and their families. Patients with JSLE will require long-term follow up. Travelling distances to tertiary services may be long and very disruptive to the child’s education and for the family. All the patients with JSLE should have shared care in place with their district local hospital and a named General Paediatrician. Patients with mild disease or who are well controlled should have the opportunity to attend part of the follow up appointments locally.UK-wide network of care for JSLE
There are few long-term outcome data on patients diagnosed with JSLE. The UK JSLE Study Group is a multi-centre, multi disciplinary collaborative network comprising representatives from nearly all the major paediatric centres in the UK providing specialist care of patients with JSLE. It has established a UK-wide cohort of patients with JSLE to improve the knowledge base of the disease. It has set standards for the assessment, diagnosis and on-going monitoring of patients with JSLE. In partnership with LUPUS UK, it is developing patient and parental information specific to JSLE and is actively pursuing a clinical trials agenda in JSLE (for more information see: https://www.liverpool.ac.uk/translationalmedicine/research/ukjsle/about/)Prof Michael W Beresford
Brough Chari, Professor of Child Health and Honorary Paediatric Rheumatologist
Department of Women's and Children's Health
Institute of Translational Medicine
University of Liverpool
Institute in the Park,
Alder Hey Children’s NHS Foundation Trust Hospital
Eaton Road
Liverpool, L12 2AP
Brough Chari, Professor of Child Health and Honorary Paediatric Rheumatologist
Department of Women's and Children's Health
Institute of Translational Medicine
University of Liverpool
Institute in the Park,
Alder Hey Children’s NHS Foundation Trust Hospital
Eaton Road
Liverpool, L12 2AP
Dr Eve Smith
NIHR Academic Clinical Lecturer
Dr Louise Oni
Senior Lecturer in Paediatric Nephrology
NIHR Academic Clinical Lecturer
Dr Louise Oni
Senior Lecturer in Paediatric Nephrology
References
1. Groot N, de Graeff N, Avcin T, Bader Meunier B, Brogan P, Dolezalova P, Feldman B, Kone-Paut I, Lahdenne P, Marks SD, et al: European evidence-based recommendations for diagnosis and treatment of childhood-onset systemic lupus erythematosus: the SHARE initiative. Ann Rheum Dis 2017, 76:1788-1796.2. Petri M, Orbai AM, Alarcon GS, Gordon C, Merrill JT, Fortin PR, Bruce IN, Isenberg D, Wallace DJ, Nived O, et al: Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum 2012, 64:2677-2686.
3. Groot N, de Graeff N, Marks SD, Avcin T, Bader-Meunier B, Brogan P, Dolezalova P, Feldman B, Kenet G, Kone-Paut I, Lahdenne P, Marks SD, McCann L, Pilkington C, Ravelli A, van Royen A, Uziel Y, Vastert B, Wulffraat N, Ozen S, *Beresford MW, *Kamphuis S (* joint senior authors). European evidence based recommendations for the diagnosis and treatment of childhood onset lupus nephritis – the SHARE initiative. Ann Rheum Dis. 2017 Sep 6. pii: annrheumdis2017-211898. doi: 10.1136/annrheumdis-2017-211898. [Epub ahead of print]. PMID: 28877866
4. Groot N, de Graeff N, Avcin T, Bader Meunier B, Dolezalova P, Feldman B, Kenet G, Kone-Paut I, Lahdenne P, Marks SD, McCann L, Pilkington C, Ravelli A, van Royen A, Uziel Y, Vastert B, Wulffraat N, Ozen S, Brogan P, Kamphuis S, Beresford MW. European evidence-based recommendations for diagnosis and treatment of paediatric Antiphospholipid Syndrome - the SHARE initiative. Ann Rheum Dis. 2017 May 4. pii: annrheumdis-2016-211001. doi: 10.1136/annrheumdis-2016-211001. [Epub ahead of print] PMID: 28473426

 ©2024 LUPUS UK (Registered charity no. 1200671)
©2024 LUPUS UK (Registered charity no. 1200671)