The Skin and Lupus
This site is intended for healthcare professionals as a useful source of information on the diagnosis, treatment and support of patients with lupus and related connective tissue diseases.
Introduction
Lupus can affect the skin in a number of different ways. Lupus presenting in the skin is referred to as cutaneous lupus erythematosus (CLE) and can occur in isolation or as part of systemic lupus. The most common skin manifestations are described below:(1)Photosensitivity: Patients report on reacting to sunlight. Classically, the rash is prominent on sun exposed areas, including but not limited to the face, back or neck, ears and chest. Sometimes care is needed to distinguish this from sunburn or a heat rash.
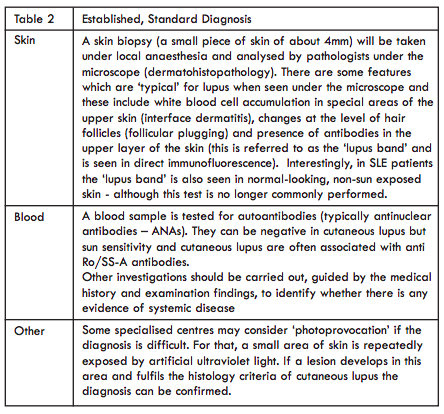
(2)Discoid lupus: Skin symptoms in the form of disc shaped, raised and red areas can occur preferentially in the face/neck/scalp areas (sun exposed locations). Skin lesions like this are referred to as discoid lupus erythematosus (DLE) (Figure 1). They often begin as small erythematosus (red) lesions which develop scaling and scaring as they enlarge. Only these types of chronic lesions commonly leave a permanent scar when healing . A scar in the scalp results in permanent hair loss in this particular area (Figure 2). If the first sign of lupus is DLE lesions, this usually does not progress to involve other organs (more than 90% of patients). However, DLE lesions can occur in patients with systemic lupus. Important differential diagnoses for newer DLE lesions include actinic keratosis, psoriasis and Bowen’s disease, whilst older DLE lesions can occasionally resemble fungal skin infections.
(3)Malar rash: Redness covering nose and cheeks is referred to as malar rash and is usually associated with SLE. This “butterfly rash” (Figure 3) may also involve the forehead, although the nasolabial folds are classically spared. Although this rash only occurs in a relatively small number of patients, it is widely recognised as a hallmark of lupus disease. Important differential diagnoses include acne rosacea, drug-induced photosensitive reactions or allergy (e.g. to cosmetics).
(4) Subacute cutaneous lupus: Skin symptoms can also present as raised circular or round red lesions and can appear in the upper trunk/forehead/arm areas. These are referred to as subacute cutaneous lupus erythematosus (SCLE) (Figure 4). These skin lesions can often be difficult to recognise and are often confused with other skin diseases (notably psoriasis, tinea corporis/fungal skin infection and pityriasis rosea).
Other less common skin lesions include:
Lupus profundus: This can be considered a deep variant of DLE with inflammation of the subdermal skin and subcutaneous fat (panniculitis). These typically painful lesions can lead to significant fat atrophy and scarring.
Lupus tumidus: A markedly photosensitive condition which often occurs in isolation without evidence of systemic disease. The lesions are typically oedematous and can resolve spontaneously, without scarring.
Figure 1. Discoid lupus erythematosus
Figure 2. Scarring alopecia
Figure 3. The typical annular rash of SCLE
Figure 4. "Butterfly" rash



Alopecia: Hair loss is common in SLE and is a frequent manifestation of a flare of systemic disease. Typically the hair loss is diffuse, and can be temporary, improving as the disease is controlled. The exception is DLE affecting the scalp. DLE lesions in the scalp often present with red/inflammatory-looking lesions which heal with scarring, resulting in permanent patchy hair loss.
Chilblain lupus: This is a relatively rare skin manifestation characterised by red/purple popular lesions, typically at the ends of fingers and toes, precipitated by cold. Longstanding lesions can result in atrophy and scarring. Lesions may be associated with pain or burning sensations. Vasodilators are often helpful in combination with steroid or immunosuppressant therapy.
It is important to remember that patients with SLE may also develop a number of non SLE-specific skin lesions including urticaria, calcinosis cutis and symptoms due to vascular phenomena (e.g. Raynaud’s syndrome).
Chilblain lupus: This is a relatively rare skin manifestation characterised by red/purple popular lesions, typically at the ends of fingers and toes, precipitated by cold. Longstanding lesions can result in atrophy and scarring. Lesions may be associated with pain or burning sensations. Vasodilators are often helpful in combination with steroid or immunosuppressant therapy.
It is important to remember that patients with SLE may also develop a number of non SLE-specific skin lesions including urticaria, calcinosis cutis and symptoms due to vascular phenomena (e.g. Raynaud’s syndrome).
How to diagnose cutaneous lupus
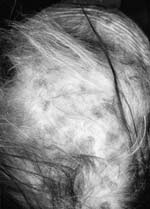
The symptoms described by the patient will give the clinicians important information (Table 1). The following are often reported by patients: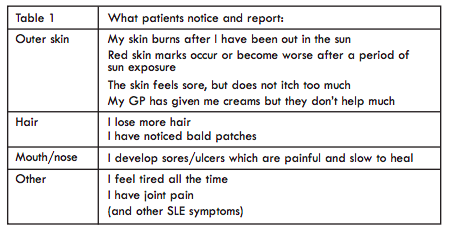
If cutaneous lupus is considered as a potential diagnosis by the clinician, the following investigations (Table 2) are usually performed, especially when skin disease is the first presentation:
The diagnostic aims are:
- To verify lupus skin inflammation
- To exclude or understand the degree of involvement of other organs (e.g. joints, kidney, blood).
- To verify lupus skin inflammation
- To exclude or understand the degree of involvement of other organs (e.g. joints, kidney, blood).
What is new regarding diagnosis?
The current ‘gold standard’ for diagnosis is the histology assessment of a skin biopsy. This requires a very small piece of skin to be taken out from a skin lesion. Unfortunately, these lesions are often on the face or on the scalp – not always the best locations for a biopsy.There are currently efforts to find non invasive (e.g. skin does not need to be cut out) ways to accurately diagnose cutaneous lupus. One such approach is to pluck out some hair follicles and to analyse the ‘root of the hair’. This method seems to work well but needs further validation in clinic.
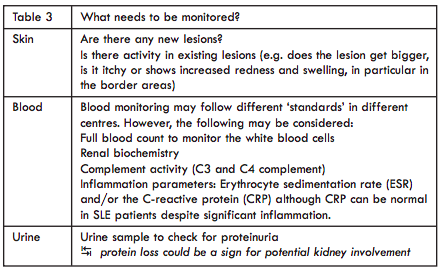
All patients with cutaneous lupus should have regular monitoring guided by the severity of the disease, presence of systemic features and any monitoring requirements specific to the treatments used (Table 3).
Assessment of lupus skin disease
It is important that lupus skin disease can be reliably documented in order to identify flares and to assess the response to treatment. In clinical trials, the Cutaneous Lupus Erythematosus Disease Area and Severity Index (CLASI) score is often used. Skin lesions are scored both in terms of activity and damage, and quantified by the area of the skin affected (e.g. arm, leg, back). The scalp is similarly scored (by quadrants) in terms of alopecia and scarring. The CLASI score offers an opportunity to quantify (as a number) the extent of skin activity and damage.Treatment
It is recommended that all patients with any type of cutaneous lupus avoid direct sunlight exposure (or other sources of ultraviolet (UV) light such as sunbeds). It is well known that both UVA and UVB radiation from sunlight can trigger a flare in the skin. In some patients, UV exposure can also cause a systemic flare of lupus. Patients should be advised to avoid direct sunlight were possible and to wear appropriate clothing. Sufficient amounts of sunscreen (2mg/cm2) with a high sun protection factor (i.e. SPF 50) should be applied 20-30 mins prior to exposure to sunlight. In rare circumstances some patients are also photosensitive to light from the visible range of the spectrum. In these patients, reflectant sunscreen containing zinc oxide and titanium dioxide (which is available in 3 colours: coffee, coral and beige) can be helpful.Note: due to avoiding sunlight exposure the skin may not generate enough vitamin D over the summer months. Vitamin D replacement therapy should be considered in all patients.
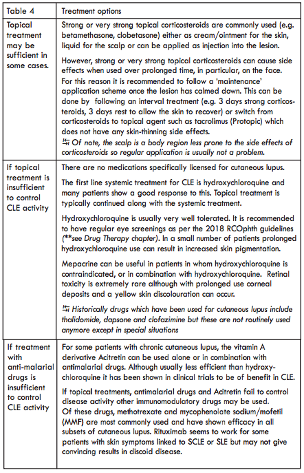
It is recommended that all patients with SLE stop smoking. Those patients who smoke often show higher disease activity and a poorer response to treatment. The principles of management of lupus skin disease are summarised in Table 4.
Conclusions
Lupus can affect the skin in a number of ways, both in isolation and as part of systemic disease. Although a number of treatment options are available, these are mostly unlicensed medications. There are currently a number of therapeutic approaches under development, efforts underway to better assess if a skin lesion is active or not and studies examining non-invasive alternatives to skin biopsy.Dr Miriam Wittmann
Associate Professor in Inflammatory
Skin Diseases
NIHR Biomedical Research Centra (BRC)
Chapel Allerton Hospital
Leeds, LS7 4SA
Dr John Reynolds
Senior Lecturer and Honorary
Consultant Rheumatologist
City Hospital
Sandwell and West Birmingham Hospitals NHS Trust
Birmingham, B18 7QH
Associate Professor in Inflammatory
Skin Diseases
NIHR Biomedical Research Centra (BRC)
Chapel Allerton Hospital
Leeds, LS7 4SA
Dr John Reynolds
Senior Lecturer and Honorary
Consultant Rheumatologist
City Hospital
Sandwell and West Birmingham Hospitals NHS Trust
Birmingham, B18 7QH

 ©2024 LUPUS UK (Registered charity no. 1200671)
©2024 LUPUS UK (Registered charity no. 1200671)