The NHS Autumn 2024 COVID-19 booster vaccination scheme is starting across England, Scotland, Wales and Northern Ireland. Eligible individuals will be able to get a booster vaccination at GP surgeries, some pharmacies and vaccination centres.
- If in England, you can book your booster vaccination online or by calling 119.
- If in Scotland, you will be invited for your booster vaccination by text, email, or letter.
- If in Wales, you will be contacted with an appointment invitation.
- If in Northern Ireland, you should contact your GP surgery or pharmacist to get your booster vaccination.
What is a booster vaccination?
A booster vaccination is a vaccination that is given after an initial vaccination. It helps to maintain an immune response to an infectious illness. In the case of COVID-19, the booster vaccination helps to provide increased protection against complications and severe symptoms of COVID-19.
 Who is eligible?
Who is eligible?
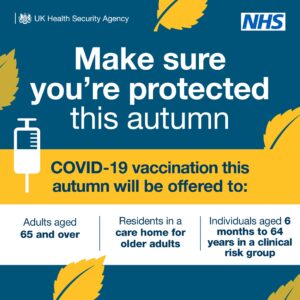
- Adults aged 65 years and over
- Residents in a care home for older adults
- Individuals aged 6 months to 64 years in a clinical risk group
- Frontline NHS and social care workers, and those working in care homes for older people
For more information on who falls into a clinical risk group, see the COVID-19 chapter of the Green Book.
Many people with lupus will qualify for their COVID-19 booster vaccination under this ‘clinical risk group’ category, however it does depend on the medications you take and the specific symptoms you have. If you have not been invited for your booster vaccination and think you are eligible, talk to your rheumatology team.
Are household contacts eligible for a booster vaccination?
Previously, household contacts of those with immunosuppression have been included in the booster vaccination programmes.
For the Autumn 2024 booster vaccination scheme, the eligibility for household contacts varies across the nations of the UK.
- England – household contacts not eligible
- Scotland – household contacts not eligible
- Wales – household contacts eligible if they are an unpaid carer. See this NHS Wales page which confirms eligibility for unpaid carers.
- Northern Ireland – household contacts not eligible
Why do I need a booster vaccination?
As we move into autumn and winter, respiratory illnesses like flu and COVID-19 start to spread a lot more around populations. This means that people will start to catch these illnesses and potentially become unwell.
COVID-19 booster vaccinations at this time of year help to provide extra protection against severe symptoms and complications, including hospitalisation due to COVID-19. If you are part of one of the clinical risk groups, you may already be at an increased risk of these complications, so a booster vaccination can help alleviate some of this risk.
There is some evidence that repeated doses of the vaccination can offer better protection for people who are immunosuppressed. This is why people who are immunosuppressed are specifically invited to have booster vaccines.
The UK Health Security Agency found last autumn (2023) that those who received a COVID-19 vaccination were approximately 45% less likely to be admitted to hospital with COVID-19 infection from 2 weeks following the vaccination, in comparison to those who remained unvaccinated.
Which vaccines are being used for the Autumn 2024 booster vaccinations?
This year, the vaccines being used as made by Pfizer or Moderna. The COVID-19 vaccine created by Pfizer is called Comirnaty, and the vaccine created by Moderna is called Spikevax.
It does not matter if you have been given different COVID-19 vaccines previously – it is safe to receive either of these vaccines.
If you cannot receive Moderna or Pfizer vaccines, there is another vaccine that can be offered through specialist services, called Novovax. You can read about this alternative vaccine here. This vaccine must be administered at a specialist clinic – if you think you may need this vaccine due to a previous adverse reaction to a COVID-19 vaccine, talk to your GP about being referred to this service.
Children under 12 years old who are eligible for booster vaccination will receive a small dose of vaccine compared to adults. In the UK, children are given the vaccine made by Pfizer.
Are the booster vaccinations safe for people with lupus?
Vaccinations can be a difficult topic to navigate if you have lupus. The COVID-19 booster vaccination is generally safe for people with lupus to receive.
If you have any concerns about receiving the vaccination, you can talk to your rheumatology team or GP team.
Our online community forum is full of discussions on various topics, including people’s experiences of vaccinations. Visit the forum here.
I would also like to have my annual flu vaccine – can I get both flu and COVID-19 vaccines at the same time?
It is generally recommended that people with lupus should have the annual flu vaccine. In a lot of GP surgeries, pharmacies and vaccine centres, they will offer both vaccines in the same appointment – this is completely safe, and does not affect how either vaccine works. If given at the same time, the healthcare professional giving the vaccine will give them in separate arms.
If you would like to have the vaccines at different times, this is also okay. You can request to have them separately and book two different appointments.
Are there any side effects for a COVID-19 booter vaccination?
You may experience minor side effects after receiving your COVID-19 booster vaccination. These side effects include:
- A sore arm at the site of the injection
- Tiredness
- Headache
- Feeling achy
- Mild flu-like symptoms
The above side effects can be managed with rest and paracetamol (use appropriate dosage as per packaging), if this is something that is normally safe for you to take. The minor side effects of COVID-19 vaccinations normally last less than a week. If you find your symptoms do not go away, or you become more unwell, contact your GP or NHS 111 for further support.
Serious side effects from COVID-19 vaccination are rare. You will be asked to wait for a while after being vaccinated so the staff there can make sure that you don’t suffer any adverse effects. Anaphylaxis (serious allergic reaction) rarely occurs after COVID-19 vaccination. If it does occur, it happens within minutes of the vaccine being administered, so staff will be there for immediate treatment.
A very rare side effect of COVID-19 vaccination is myocarditis and pericarditis. This is inflammation of the heart. The symptoms include chest pain, breathlessness and palpitations. If you experience these symptoms, seek medical attention. Episodes of this after COVID-19 vaccination are typically mild with a short recovery time.
If you do experience side effects from your COVID-19 vaccine, you can report them via the Yellow Card Scheme.
If you experienced significant side effects or an adverse reaction to previous COVID-19 vaccinations, get in contact with your healthcare team or GP to discuss what is best for you.
Should I have the booster vaccination if I am unwell or experiencing a lupus flare?
If you are experiencing a lupus flare, get in contact with your rheumatology team to discuss whether now is the right time to receive your COVID-19 booster vaccination.
If you are unwell, you should wait until you are recovered to receive your COVID-19 booster vaccination.
If you have a fever, or think you may be infectious, please do not attend your vaccination appointment, and reschedule for when you are recovered.
I had an adverse reaction to a previous dose of the vaccine, should I have the booster?
If you experienced significant side-effects or an adverse reaction from any previous dose of the COVID-19 vaccine, speak to your healthcare team to discuss what may be best for you.
According to the JCVI Green Book, there are very few individuals who cannot receive the vaccine. Following careful monitoring of the vaccine rollout, they have issued specific guidance for those with allergies and those who have had an allergic reaction to a previous dose of the vaccine. Your healthcare team will follow this guidance and can discuss the options with you.
I am on immunosuppressive medication – can I have my COVID-19 booster vaccination?
In the UK, all COVID-19 vaccines used are safe for people with suppressed immune systems.
Immunosuppression may affect the effectiveness of the COVID-19 vaccination. However, it is still recommended that those who are immunosuppressed receive their booster vaccinations, as there is some evidence that repeated doses can help provide better protection.
If you are concerned about the effect of immunosuppression on your ability to have the COVID-19 booster vaccination, contact your healthcare team via phone or email to find out more.
Some examples of immunosuppressive medications include:
- Azathioprine
- Methotrexate
- Leflunomide
- Mycophenolate
- Ciclosporin
- Tacrolimus
- Sirolimus
- Cyclophosphamide
Biologic medications such as rituximab, belimumab and anifrolumab also suppress the immune system.
Hydroxychloroquine is not classed as an immunosuppressant.
Further information:
You can find further information about the COVID-19 vaccine programme: